| Seguici su Facebook.com/AmygdalaPanicDisorder - - - - - - (C) 2015/2016 GRAZIE A PUBMED.GOV |

|
|
 |
 |
| Cos'è un Attacco di Panico? Amigdalectomia Evoluta: minor tessuto, minor rischio Scoperte scientifiche |
| Indice Istituzionale Chi siamo e Motivazioni Le Definizioni Epidemiologia I diritti del Paziente |
|
(italiano, breve sintesi) * Agorafobia: insopprimibile ed abnorme paura degli spazi aperti, dipendenza dalle mura domestiche con importante perdita delle attività lavorative e sociali; * Disturbo di Panico: episodi ricorrenti di terrore seguiti da cambiamenti comportamentali disabilitanti dovuti dalla incontrollabile preoccupazione (conscia e/o inconscia) di avere altri attacchi; Alcuni sintomi comuni di un attacco includono sudorazione, capogiri e vertigini, dispnea, tremore, pulsazioni instabili, pensieri incontrollabili come paura di perdere il controllo o impazzire, paura di morire e iperventilazione. Altri sintomi sono paralisi ed eccessiva contrazione muscolare, dolori corporei, nausea, addormentamento e/o formicolio, freddo improvviso, bruciori, debolezza, pianto, disperazione, percezione alterata della realtà. Il DSM-V separa il disturbo di ansia da quello di panico, in quanto quest'ultimo si manifesta in modo più acuto e traumatizzante. * PTSD: condizione cronica di stress, ansia, stanchezza, problemi di memoria e cognitivi, difficoltà di riposo e sonno (malfunzionamento del sistema parasimpatico). Tale condizione emerge solitamente da "eventi traumatici" (guerre, violenza, incidenti, attacchi di panico, ..) o da "forti, prolungate situazioni di stress" o entrambe le cose concorrenti. Definitions: Agoraphobia - Insuppressible and abnormal fear of opened spaces, dependency from closed spaces or house walls, with consequent loss of work and social relationships. In intermediate cases the person is able to leave home accompained by trusted people, in slight cases the panic is limited to specific cicrumstantial zones (fields, streets, squares, supermarkets, bridges, airports, ..). Collateral diseases, like depression, PTSD, anxiety, bipolar disorder associated with rage, impulsiveness and aggressiveness, sleep disturbance, addiction, gastrointestinal disease and general bad health, .., are frequently associated. ...... Definitions: Panic Disorder - A disorder characterized by recurring Panic Attacks, causing a series of intense episodes of extreme fear and terror. Panic Disorder also include significant disabling behavioral changes due to the worries (conscious and/or unconscious) of having other attacks. Some common symptoms of an attack include rapid heartbeat, perspiration, dizziness, dyspnea, trembling, uncontrollable feelings such as the fear of losing control and going crazy, the fear of dying and hyperventilation. Other symptoms are sweating, a sensation of choking, paralysis, chest pain, nausea, numbness or tingling, chills or hot flashes, faintness, crying and some sense of altered reality. Individuals suffering from an episode have a strong wish of escaping from the situation that provoked the attack. The Panic Disorder is particularly severe compared to Generalized Anxiety Disorder. The DSM-V describes panic disorder and anxiety differently, panic attacks are acute events triggered by a sudden, out-of-the-blue cause: duration is short and symptoms are more intense. ...... Definitions: Post Traumatic Stress Disorder - PTSD is a chronic mental condition emerging from "traumatic events" (war, violence, accident, panick attack, ..) or "strong, prolonged stress" or both mixed together. Symptoms may include stress, tiredness, cognitive and memory problems, resting and sleep difficulties (parasimpatetic failure), nightmares, flashbacks, panic or severe anxiety, as well as uncontrollable thoughts. In PTSD patient avoids certain places, people, behaviors or thoughts, pictures or sounds (stressors) to not suffer. PTSD is categorized in DSM-5 as "trauma and stress-related disorder" and considered chronic when persisting for over three months. Major areas involved in PTSD are PFC (prefrontal cortex), amygdala and insula. |
|
fig.1: circuit of pathological fear - simplified schematic view (based on LeDoux's studies) 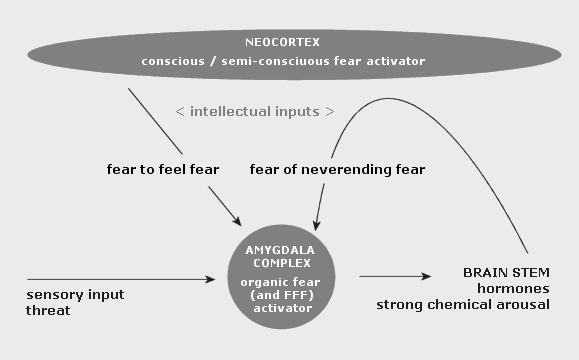
|
|
fig. 2: model for the development of fear-related disorders (Parsons et al., Nature Neuroscience 16 / 2013)  
Certain individuals are predisposed to the development of fear-related disorders on the basis of early life experience and genetic background, among other risk factors. When a traumatic event occurs, people learn to fear the cues that are associated with the traumatic event, and this memory consolidates over the course of the subsequent hours and days. The expression of fear comes in several different forms, including flashbacks of the traumatic event, nightmares, avoidance of situations that trigger memory for the traumatic event and altered sympathetic responses such as increased startle. Additionally, fear may generalize to cues not associated with the initial traumatic event in those people who go on to develop a fear-related disorder. |
condividi:
STAMPA QUESTA PAGINA

|
|
| AMYGDALA.LINK (C) 2015/2016 ARR - - - - - - Un RINGRAZIAMENTO speciale a Paternita.info e PubMed.gov |